What do I need to know about cataracts?
The human eye is similar to a camera, capturing light to form an image that is then ‘seen’ by the brain. Just like in a camera, there is a lens inside the eye that serves to focus light from the outside world. When we are born, this lens is crystal clear, and light can get through easily, forming a sharp, clear image. However, as we age, the lens naturally begins to cloud and become milky. This milky lens is called a cataract.
Sunlight, diabetes, smoking, and certain drugs can speed up this process, as can injury or eye surgery. Light can’t pass through a milky lens easily, and the world looks blurry and dim as a result. Many people also find glare to be a problem, especially when driving at night, or that colours aren’t as bright and vivid as they used to be. There are no medicines or drops that can treat cataracts, but they can be corrected with a short surgery that removes the cloudy lens and replaces it with a clear artificial one, restoring vision. Untreated, cataracts will steadily progress, making vision worse and worse. Cataracts are incredibly common (everybody will get them eventually), and more cataract surgeries are done in Canada each year than any other kind of operation.
What do I need to know about cataract surgery?
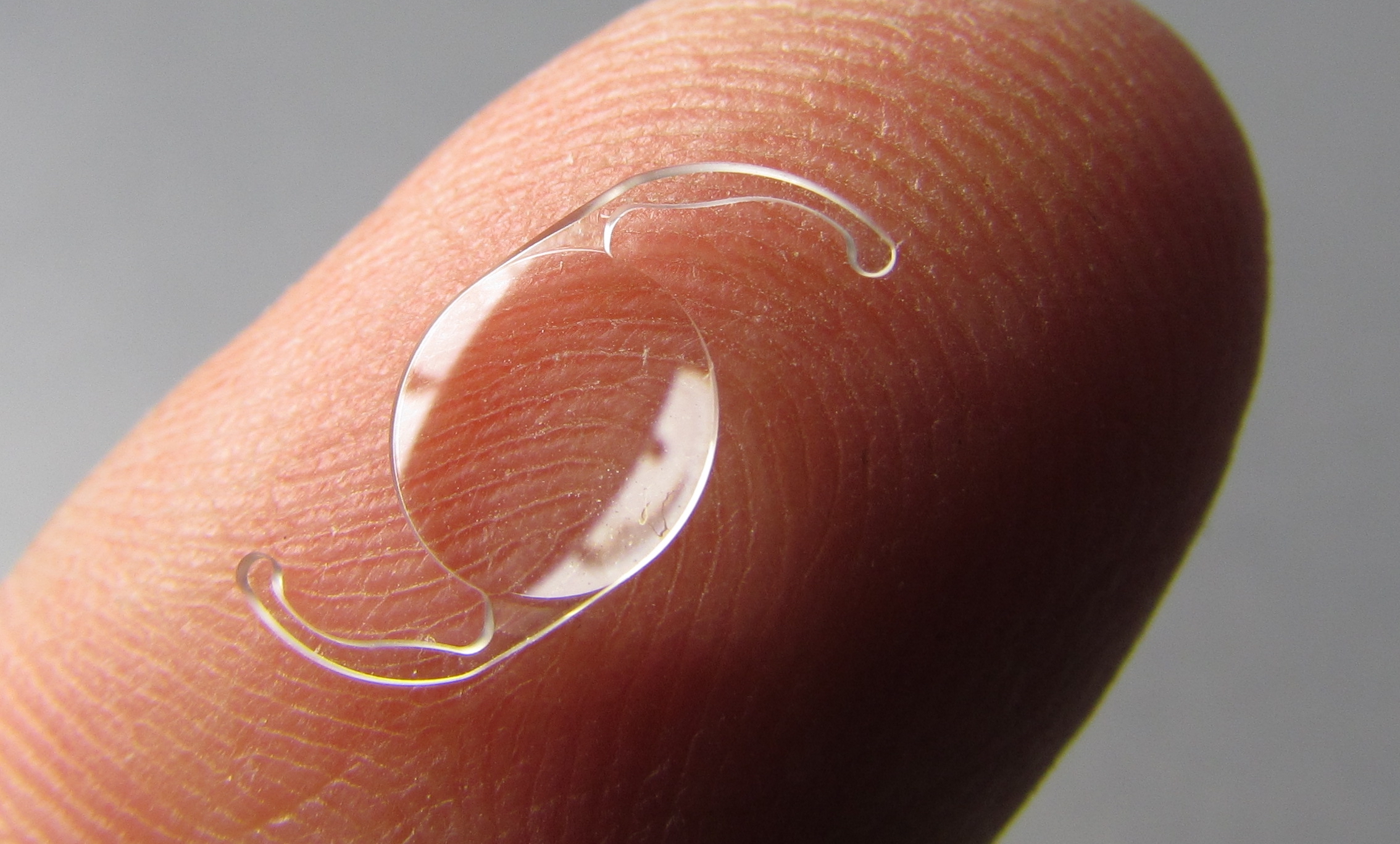
Cataract surgery removes the milky lens that is blocking light from entering the eye and replaces it with an artificial (plastic) lens that will never get cloudy or milky. Your surgeon may refer to this artificial lens as an ‘intraocular lens’, or IOL. Your ophthalmologist will recommend surgery when the cataracts are severe enough that they impact your quality of life. Cataract surgery generally takes less than 20 minutes, and can usually be done without the need for general anesthesia (being put to sleep). Depending on where you live, surgery may happen in a hospital, or in a surgery centre.